This Black History Month, to amplify Black voices and foster meaningful conversations around Black mental health, Grant Halliburton Foundation is highlighting staff and board members who are driving positive change at the Foundation and throughout North Texas.
Today, we're spotlighting Yvonne Merritt, mental health education manager, to explore her experiences, insights, and contributions in creating a more inclusive, equitable, and mentally healthy world for the Black community.
How are you involved and impacting the Black mental health community in North Texas?
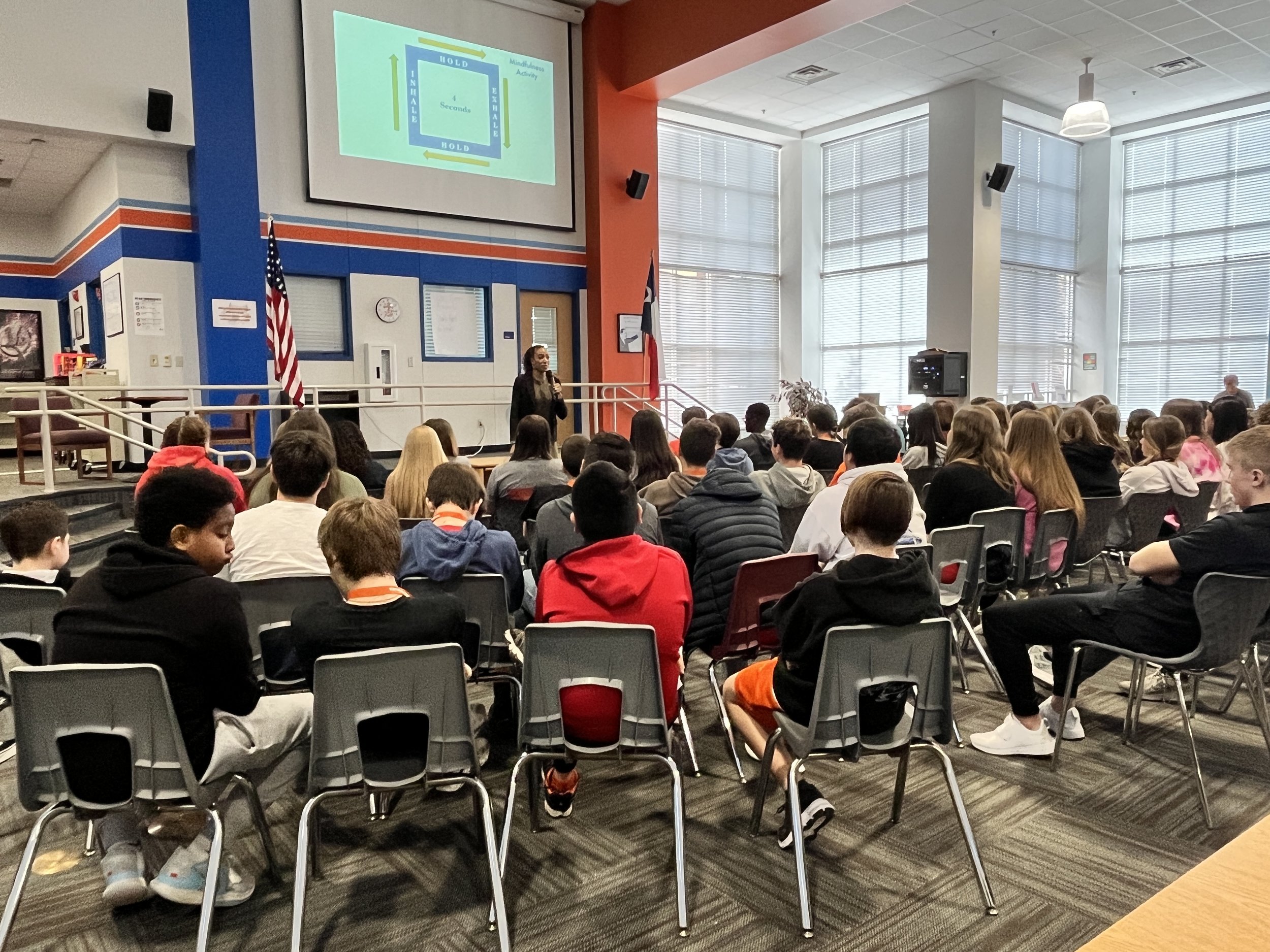
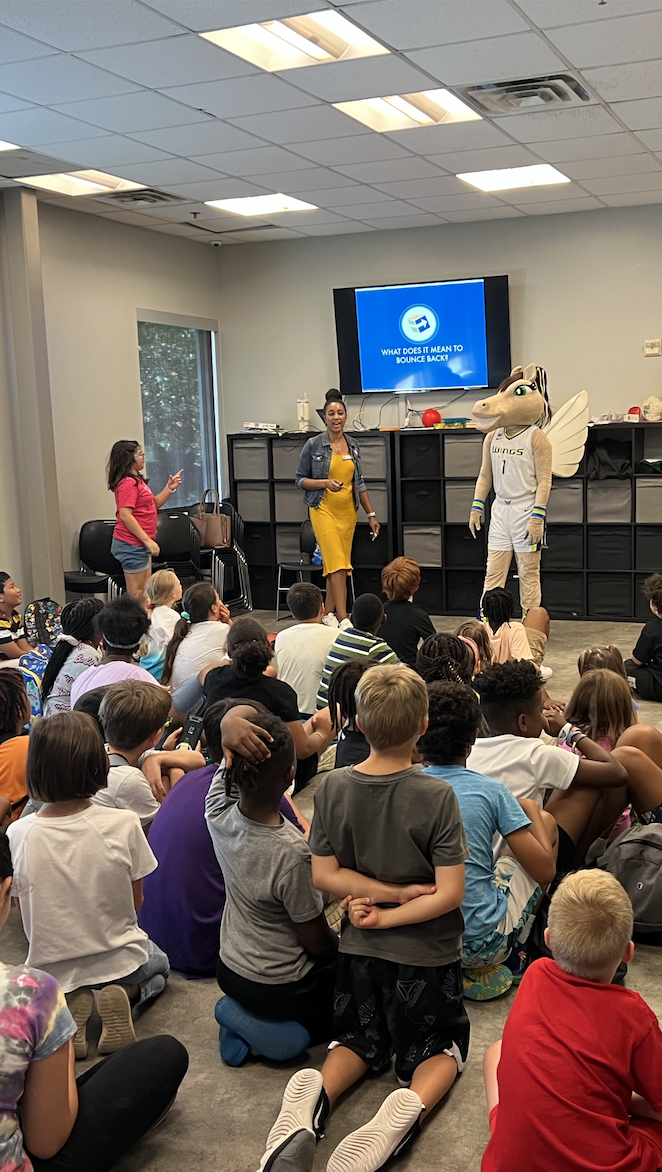
My involvement in the Black mental health community in North Texas has been both meaningful and transformative. As a mental health education manager with the Thrive Education team, I speak to students, parents, guardians, teachers, and staff to educate them about mental health. In collaboration with local schools and community organizations, Grant Hallibuton Foundation presents a mental health education program that specifically addresses the challenges faced by youth.
We’ve been expanding our reach to support communities that have larger barriers to mental health resources and that largely includes Black youth. By engaging with educators, parents, and students, we've been able to create a more inclusive and supportive environment that promotes mental well-being from an early age. However, I recognize there’s still much work to be done. My ongoing commitment involves expanding our outreach, collaborating with other school districts and organizations, and advocating for policies that address the systemic issues affecting mental health in the Black community.
When Black History Month is mentioned, what thoughts and sentiments come to mind for you personally, particularly about mental health?
When Black History Month alone is mentioned, my thoughts immediately turn to reflection and celebration of the rich contributions, resilience, and achievements of the Black community throughout history. In relation to mental health, Black History Month serves as a reminder of the importance of acknowledging and addressing the unique mental health challenges that individuals in the Black community may face. Black History Month encourages conversations around mental health that are intersectional and inclusive. It prompts us to recognize and address the unique socio-cultural factors that influence mental health experiences within the Black community. It's a time to celebrate the achievements and milestones, but also to acknowledge the ongoing work needed to create a more equitable and supportive environment for mental well-being.
What specific mental health issues do you find most prevalent or pressing within the Black community, and how do you address them in your work?
The black community is more likely to experience economic distress, racism, and other social circumstances that increase their chances of developing depression or other mental illnesses. According to Substance Abuse and Mental Health Services Administration (SAMHSA), 13.4% of the U.S. population identify as Black or African American. Of those, more than 16% reported having a mental illness in the past year. That is more than 7 million people! To think that this is only those who have reported having a mental illness is alarming.
here are Black youth who are still struggling with overwhelming amounts of stress and emotions that send them into a depressed state. Depression effects every person differently, but according to the CDC, in the Black community, the rate of severe depressive symptoms along with mild to moderate depressive symptoms are higher than white counterparts. It’s important that the Black community knows that depression is a treatable medical condition. Although we can’t pinpoint what the cause may be, we can combat depression with therapy, self-help strategies, coping skills for stress, and medication circumstances permit.
“Depression effects every person differently, but according to the CDC, in the black community the rate of severe depressive symptoms along with mild to moderate depressive symptoms are higher than white counterparts. It is important that the black community knows that depression is a treatable medical condition.”
As a professional in the mental health field, how do you work to dismantle stigmas surrounding mental health in the Black community?
Historically, stigma and judgment prevent the Black community from seeking treatment for their mental illnesses. Research indicates that Black people believe mild depression or anxiety would be considered “crazy” in their social circles. Some even fear speaking about it to close friends or family. To break this stigma, I plan to continue cultivating spaces where black voices can be heard and respected. We can do this by requiring education to normalize conversations about mental well-being. The Foundation’s Thrive Education programs can help by continuing to educate teachers and staff, community members, and parents on how to incorporate mental health and well-being practices into the day-to-day schedules of youth. Creating safe spaces allows Black students to feel more welcome to share their mental health concerns.
How can mental health professionals better cater their services to be more inclusive and culturally competent for the Black community?
In the pursuit of delivering mental health services that are truly inclusive and culturally competent for the Black community, continuous cultural competence training is paramount. Fostering a nuanced understanding of the diverse backgrounds and experiences inherent within the Black community is not merely an aspiration, but a fundamental prerequisite for cultivating a mental health landscape that respects, validates, and responds effectively to the unique needs and strengths of each individual.
Mental health professionals should recognize the intersectionality of identities within the Black community, tailoring services to address unique experiences related to gender, sexual orientation, and socioeconomic status. Mental health professionals should incorporate culturally relevant therapeutic interventions. Treatment plans must be personalized, considering individual cultural backgrounds, values, and beliefs, acknowledging historical and systemic traumas is essential and implementation of trauma-informed care as needed.